You Won't Believe: Delivers Revolutionary Medical Breakthroughs in a Shocking Documentary!
Planet TV Studios displays a televised account regarding Dr. Brandon Gough's Advances in Surgical Techniques in "New Frontiers" — Showing March, 2024 via Nationwide TV and Video On-Demand.
BOCA RATON, FL, USA, March 5, 2024 / ReportWire.org -- Planet TV Studios proudly presents its fresh series of documentaries, "New Frontiers," featuring the innovative milestones by Gough Surgical, PLLC. This series navigates through the dynamic evolutions driven by Dr. Brandon Gough, M.D., an acclaimed orthopedic specialist concentrating on microinvasive methodologies and computer-assisted hip and knee replacement surgery.
"New Frontiers" serves as an engaging journey expertly crafted for highlighting revolutionary companies defining the next generation of healthcare worldwide. Set your reminder for each documentary installment premiering in Q2 2024 on the national network, Bloomberg TV, and offered on-demand on services including the Amazon service, Google Play, Roku, among others.
Planet TV Studios is honored to host Gina Grad in the role of host once more. Gina is recognized as an expert author, podcast host, and broadcast personality residing in Los Angeles, California. She has a background as the co-host and news anchor of the Adam Carolla Show, a record-breaking podcast in terms of downloads. Gina has operated as an anchor on KFI 640 AM and led morning broadcasts on 100.3 FM. She is actively hosting "The Bryan and Gina Show, The Official Podcast of LA Magazine." Beyond her work on air, she authored "My Extra Mom," a children's volume meant to assist children and non-biological parents in overcoming the issues arising in blended familial situations.
Dr. Brandon Gough, M.D., is acknowledged as a remarkably celebrated orthopedic expert, accredited and noted for his surgical excellence in replacement operations for hip and knee through the region of Phoenix, Arizona. Harnessing advanced robotic technology together with precision micro-invasive and muscle-conserving operations, Dr. Gough commits to enabling rapid recoveries towards a fast recovery into active living. His prioritization of soft tissue preservation fosters speedy recuperation, curtails hospital stays and, in specific situations, enables total joint replacement in an outpatient setting. He is known as a preeminent figure globally for the Direct Superior Approach combined with muscle-sparing robot-assisted surgery.
Recognizing education as fundamental, Dr. Gough leverages continual learning to provide first-rate patient care in Orthopedic Medicine. Once his undergraduate studies were completed at Spring Hill College located in Mobile, Alabama, he sought his medical degree at Creighton University School of Medicine situated in Omaha, Nebraska. Dr. Gough deepened his practical knowledge through residency and internship in General Orthopedics at the University of Kansas, School of Medicine in Wichita, KS, where he gained the title of Resident Teacher of the Year. He continued to specialize with a fellowship in Lower Extremity Adult Reconstruction at the Arizona Institute of Bone and Joint Disorders.
A board-certified professional of the American Board of Orthopedic Surgeons and an active participant in groups such as the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's steadfast commitment to excellence is evident beyond his medical practice. He serves as Vice President of the Orthopedic Surgery Interest Group and maintains memberships with the American Medical Association and American College of Physicians. His practice is based at the prestigious Orthopedic Institute of the West, a center he assisted in founding, and he maintains surgical privileges at Scottsdale Abrazo Hospital, Liberty Hospital, as well as select surgery centers throughout the Phoenix/Scottsdale, AZ region. Motivated by his zeal for advancing surgical methods, he directs efforts toward founding a center of excellence for robotic hip and knee replacements and extends his expertise through global surgeon training.
In addition, his strong community spirit drives him to volunteer with numerous charitable organizations including the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
Importantly, Dr. Gough acts as a consultant and instructor for Zimmer Biomet, reinforcing his dedication to progressing orthopedic care and surgical innovation.
About Planet TV Studios— Planet TV Studios designs avant-garde, reality television series featuring comprehensive updates on critical business, medical, and socially impactful subjects.
For further details regarding Gough Surgical, PLLC, visit https://goughmd.com.
For more on the series, please navigate to https://planettvstudios.com / https://planettvstudios.com/backstage/ or get in touch with Christian Alain at 888-210-4292 x100 or at christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Steering Upcoming Era of Orthopedic Care
Amid the landscape of orthopedic surgery, attention to detail, experience, and creativity converge at Gough Surgical Adult Hip & Knee, a prominent practice exclusively devoted to adult hip and knee prosthetic procedures.
With the proficient direction of Dr. James Gough, this dedicated facility has secured honors for revolutionizing patient experiences by reestablishing locomotion, curbing pain, and remarkably uplifting life standards for countless patients.
Defining New Criteria in Orthopaedic Interventions
Skeletal procedures, especially concerning the hip and knee joints, represent some of the most common procedures conducted internationally.
However, clinical success and patient satisfaction figures vary widely depending on clinical proficiency, facility quality, and the practitioner's strategy.
Gough Surgical excels by dedicating itself solely to adult hip and knee replacements, fostering concentrated know-how rare in the general industry.
Dr. James Gough, distinguished for his surgical accuracy and patient-centric attention, has spent his career perfecting these multifaceted procedures.
His clinic, Gough Surgical Adult Hip & Knee, optimally located to address the needs of patients from multiple regions, has become synonymous with exceptional outcomes, faster recoveries, and higher patient satisfaction rates.
Outstanding Quality Anchored in Focus
Why dedicate practice solely to adult hip and knee replacements?
According to Dr. Gough, exclusive practice results in unparalleled proficiency.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," notes Dr. Gough.
This specialized knowledge converts to diminished adverse events, diminished operative risks, and elevated patient satisfaction.
State-of-the-Art Surgical Approaches and Tools
Gough Surgical Adult Hip & Knee regularly integrates state-of-the-art technology to augment surgical precision and patient outcomes.
One of the prominent aspects of the clinic involves using advanced robotic operative systems.
These advanced systems facilitate incomparable exactitude, culminating in accurate placement of implants fitted to individual anatomical features.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," observes Dr. Gough.
Patient-Focused Care: Beyond a Simple Procedure
At Gough Surgical, patient support reaches further than the operating table.
From the opening consultation through comprehensive recovery check-ups, patients receive personalized, attentive care every step of the way.
This multifaceted approach promotes bodily healing and encourages emotional support and confidence across the entire treatment process.
Dr. Gough reminds us, "Recognizing the distinct requirements, anxieties, and objectives of every patient is vital." Bespoke care substantially enhances healing processes and overall patient satisfaction.
Comprehensive Pre- and Post-Operative Support
Gough Surgical’s emphasis on thorough care shows itself via its in-depth preoperative protocols and comprehensive postoperative check-ups.
Structured pre-surgery instructional courses, targeted patient training sessions, and direct consultation meetings condition patients for physical and cognitive readiness, lowering stress and spurring informed choices.
Following the operation, the facility’s systematic recuperation strategies and individualized physical therapy programs promote speedier, more fluid recoveries.
Clients favor the transparent instruction, periodic progress reviews, and uncomplicated access to seasoned advice, notably augmenting their recovery experience.
Innovative Solutions for Complex Conditions
Gough Surgical Adult Hip & Knee is renowned for its capability in resolving complex issues that other centers find demanding.
Encompassing intricate joint replacement revisions and severe arthritic cases, this practice introduces pioneering treatments by means of advanced surgical methods, minimally invasive interventions, and individualized implant designs.
These these tailored treatments typically produce rapid recovery, decreased postoperative aches, and rejuvenated movement, empowering patients to quickly reclaim an active, pain-free existence.
A Heritage of Client Contentment
The patient reviews and feedback vividly illustrate the life-changing effects of its treatment.
Patients commonly report reclaiming independence, experiencing substantial pain relief, and enjoying a superior quality of life following their operations.
"Walking without pain was something I never imagined possible again," remarks Mary Thompson, a patient treated with a complete knee replacement at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," continues Mary Thompson.
Continual Research and Professional Development
Beyond medical proficiency, Gough Surgical Adult Hip & Knee actively fuels advancements in orthopedic care with continuous research and training.
Dr. Gough regularly involves himself in research studies, contributing significant findings that boost orthopedic understanding and care protocols.
Additionally, the clinic holds regular educational events and practical workshops, nurturing collaborative learning among professionals and continuously advancing industry criteria.
A Forward-Thinking Approach to Orthopedics
As the sphere of bone and joint medicine progresses, Gough Surgical maintains its pioneering stance by regularly assimilating cutting-edge technologies and approaches.
The practice’s commitment to perpetual advancement guarantees that patients benefit from the latest, most efficient treatment modalities.
"{Our goal is to redefine what's possible in orthopedic surgery continually," remarks Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," adds Dr. Gough.
Conclusion: Pioneering the Future of Hip & Knee Care
Gough Surgical Adult Hip & Knee stands prominent in orthopedic medicine by intertwining advanced operative strategies, specialized care, and nurturing patient engagement.
By steadily advancing beyond conventional boundaries, Dr. James Gough and his focused team not only restore joint functionality—they substantially better lives.
In the endeavor for seamless movement and regained vitality, Gough Surgical Adult Hip & Knee does not only change orthopedic paradigms—it lays down new foundations for the future of healthcare.
Micro-Invasive along with Muscle-Preserving Operative Methods: Reshaping Advanced Medicine
Over recent decades, procedural innovation has reshaped clinical care, delivering minimal trauma, brisk healing, and improved outcomes.
Among these advancements, micro-invasive and muscle-sparing surgical methods have emerged as transformative techniques.
These approaches have not only reformed the intervention suite, but also redefined the patient experience.
This report delves into the evolution, techniques, benefits, challenges, and future directions of micro-invasive and muscle-sparing surgery, utilizing expert insights, clinical studies, and real-world applications.
A New Era in Surgery: The Rise of Minimally Invasive Approaches
The modern operating room is a far cry from the large incisions and extended hospital stays that characterized surgery a century ago.
Surgeons today increasingly rely on procedures that reduce tissue disturbance and preserve the body’s original design.
Key to these surgical advances are represented by micro-invasive and fiber-preserving procedures.
In micro-invasive surgery, one refers to techniques that use small incisions, specialized instruments, and high-definition imaging to access and treat internal conditions with minimal disruption to surrounding tissues.
Oppositely, fiber-preserving surgery aims at safeguarding muscle tissue integrity during operations historically associated with extensive muscle dissection.
Each technique is a facet of the overarching push to lower patient morbidity, pain, and the length of recovery.
A Look Back: Transitioning from Open Surgery to Tissue Preservation
The conduct of surgery has always been shaped by immediate needs and technological availability.
Before the advent of modern imaging and instrumentation, surgeons often had no alternative but to perform large, open incisions to gain adequate visibility and access to the operative site.
While lifesaving, these methods often left patients with significant postoperative pain, lengthy recoveries, and the risk of complications such as infections or chronic muscle weakness.
The evolution initiated with laparoscopic surgery’s development in the late twentieth century—a minimally invasive method that facilitated internal observation with a small camera inserted via limited incisions.
As advancements in technology unfolded, surgical teams realized that conserving muscle integrity during operations could bring additional benefits.
Muscle-sparing techniques, initially developed in orthopedics and cardiovascular surgery, soon found applications in abdominal, gynecological, and oncological procedures, among others.
Dr. Eleanor Matthews , a pioneer in minimally invasive approaches at a respected teaching hospital, affirms: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This adoption of less invasive methods not only represents a technical achievement but also a profound change in the philosophy of surgical care.
Foundational Science Underpinning the Techniques
Micro-Invasive Surgery: Precision Through Technology
At the core of micro-invasive surgery is the principle of precision.
Surgeons use an array of high-tech tools—from endoscopes and robotic-assisted devices to specialized microscopes—to navigate the human body through minuscule openings.
These instruments provide enhanced magnification and illumination, enabling the precise identification and treatment of the target area without extensive tissue damage.
A major breakthrough has been the incorporation of robotic-assisted surgical platforms.
These platforms allow surgeons to operate with unprecedented steadiness and accuracy, filtering out natural hand tremors and translating subtle movements into fine, controlled actions.
In procedures such as prostatectomies and cardiac surgeries, this precision translates directly into improved patient outcomes.
Cardiothoracic Surgery: Minimizing Cardiac Trauma
Cardiothoracic surgery has also benefited significantly from micro-invasive methods.
Procedures such as valve repairs and coronary artery bypass grafting (CABG) have traditionally required large incisions and extensive dissection of muscle tissue.
Today, surgeons increasingly employ minimally invasive techniques that use small incisions and specialized instruments to access the heart and surrounding structures.
The adoption of robotic-assisted systems in cardiothoracic surgery has further refined these procedures.
In many cases, the robotic platform provides the precision required to perform delicate maneuvers on the beating heart, reducing the risk of complications and promoting faster recovery.
A comparative study published in the Annals of Thoracic Surgery found that patients undergoing minimally invasive valve repairs had lower rates of postoperative atrial fibrillation and shorter hospital stays compared to those who underwent conventional surgery.
General and Gynecologic Surgery: Enhancing Patient Outcomes.
Within general and gynecologic practices, minimally invasive methods have transformed interventions like gallbladder removals, hernia repairs, and hysterectomies.
This transition to limited incisions and muscle conservation not only diminishes visible scarring but also lessens postoperative pain and the likelihood of complications.
For instance, laparoscopic cholecystectomy—removal of the gallbladder through small incisions—has become the standard of care in many parts of the world.
Those undergoing the procedure enjoy shorter healing times and nearly immediate return to normal activities.
In gynecology, muscle-sparing techniques have been instrumental in improving outcomes for women undergoing complex procedures such as myomectomies or pelvic floor repairs.
A leading medical journal’s review of clinical outcomes found that minimally invasive gynecologic surgeries lead to lower infection and blood loss rates, as well as superior cosmetic outcomes.
These improvements not only enhance patient satisfaction but also contribute to better overall health outcomes.
Weighing the Benefits and Challenges.
Benefits That Extend Beyond the Operating Room.
The gains from minimally invasive and muscle-sparing approaches extend far beyond the technical realm of surgery.
For patients, the outcomes are noticeable and significantly transformative.
The reduction in pain, scarring, and recovery time directly translates into a better quality of life.
For many, the possibility of returning to work and normal activities within days, rather than weeks, is a key benefit in a fast-paced society.
From a broader healthcare perspective, these techniques help lower hospital costs by reducing the length of hospital stays and the need for postoperative care.
Additionally, fewer complications mean fewer readmissions, which is a significant consideration for healthcare providers and insurers alike.
Psychological gains must not be disregarded.
Understanding that a surgery can be conducted with little bodily impact offers comfort and lowers preoperative stress.
This element is particularly significant for those facing extensive surgeries, with a calmer and positive perspective aiding better overall outcomes.
Challenges and Limitations: A Realistic Perspective.
Despite the numerous advantages, micro-invasive and muscle-sparing techniques are not without challenges.
A prominent drawback is the steep learning curve tied to these advanced techniques.
Surgeons must undergo rigorous training and gain substantial experience before they can perform these procedures with the same level of proficiency as traditional surgeries.
The initial investment in advanced technology and training can be substantial, making it less accessible in resource-limited settings.
Also, these approaches are not universally applicable to all patients.
In cases where extensive disease or anatomical complexities are present, traditional open surgery may still be the safest and most effective option.
Every case demands careful evaluation by surgeons to balance the benefits of minimally invasive approaches against the individual needs of the patient.
Technical limitations also play a role.
Even with cutting-edge technology, limitations in the operative field or sudden complications may necessitate converting to a traditional open approach.
While uncommon, these cases highlight why it is essential to have a versatile and adaptive surgical team.
Expert Insights and Patient Perspectives
Voices from the Frontline
Dr. Michael Andersen, a renowned surgeon with 25+ years of experience in minimally invasive procedures, asserts the importance of personalized care
“Every patient is unique, and while micro-invasive and muscle-sparing techniques offer tremendous benefits, the key is to tailor the approach to the patient’s specific condition and overall health,” he explains.
His insights underscore a fundamental tenet of modern medicine: technology must serve the patient, not dictate the treatment plan.
In a similar vein, patients treated with these methods regularly mention the significant, transformative effects on their day-to-day living.
Maria Lopez, a 54-year-old patient who recently experienced a muscle-preserving breast reconstruction, shares her personal story.
“I was ready for a drawn-out, painful recovery; however, I was up and active within days, feeling as though I had been reborn,” she remarks.
Such testimonials, while anecdotal, are supported by robust clinical data that points to improved outcomes with these techniques.
Building a Trustworthy Surgical Ecosystem.
The increasing acceptance of minimally invasive and muscle-preserving techniques is driving a widespread cultural transformation in healthcare.
Surgeons, hospitals, and educational initiatives are uniting to share best practices, create standardized guidelines, and commit to ongoing research.
Regularly organized conferences and symposiums on minimally invasive techniques now serve as vital forums for expert discussion on innovations, obstacles, and future prospects.
This collaborative approach is essential for addressing the challenges associated with these advanced techniques.
By pooling expertise and resources, the medical community is better positioned to refine surgical methods, reduce complications, and ensure that the benefits of these techniques are accessible to a wider population.
Next-Generation Surgery: Trends, Innovations, and Transformative Approaches.
Adopting AI-Enabled and Robotic Approaches.
While current micro-invasive and muscle-sparing techniques have already made a profound impact, the future promises even more dramatic changes.
Integrating AI and machine learning into surgical technologies promises to augment accuracy and efficiency.
These technologies can analyze vast amounts of data in real time, offering surgeons predictive insights that may improve decision-making during complex procedures.
For example, AI-powered imaging systems are being developed to automatically highlight critical anatomical structures, reducing the risk of inadvertent injury.
Additionally, robotic platforms are evolving, with state-of-the-art systems offering enhanced precision and haptic feedback, allowing surgeons to experience tactile sensations of the tissue—a feature lacking in traditional laparoscopic devices.
Expanding the Parameters of Minimally Invasive Surgery.
Research and development in the field of tissue engineering and regenerative medicine are likely to intersect with surgical innovations.
Scientists are exploring ways to not only minimize tissue damage but also promote faster, more natural healing.
This includes the use of bioengineered scaffolds that can support tissue regeneration and reduce scar formation after surgery.
Moreover, as imaging and sensor technology continue to improve, surgeons may be able to perform procedures that are even less invasive than those currently available.
Future innovations such as nanorobots and micro-implantable devices might one day permit targeted therapy and diagnostics at a cellular level, marking the onset of a new epoch in personalized medicine.
An International Standpoint: Narrowing the Divide in Surgical Services
While state-of-the-art innovations are reshaping surgical practices in affluent regions, significant disparities in the availability of advanced surgical care continue to exist worldwide
Addressing this chasm demands concerted collaboration between public institutions, non-governmental organizations, and the international medical arena
Professional development programs, technology dissemination efforts, and allied research collaborations are essential to provide global patients access to state-of-the-art micro-invasive and muscle-sparing treatments
International cooperative efforts are yielding positive outcomes
Facilities in affluent nations are collaborating with medical centers in emerging areas to offer instruction and assistance in state-of-the-art, minimally invasive procedures
Such partnerships improve patient outcomes while simultaneously fostering a more equitable and robust global healthcare system
Plotting the Road Ahead: Barriers and Future Opportunities
The march toward comprehensive use of cutting-edge micro-invasive and muscle-preserving surgery is impeded by a range of challenges
The financial outlay needed for advanced technological tools, together with the requirement for dedicated training, is significant
Yet, the long-term benefits, including enhanced patient results and significant cost savings in healthcare, imply that these challenges are surmountable
Healthcare decision-makers are increasingly aware that investing in innovative surgical methods can deliver impressive returns
Reduced hospital stays, diminished rates of complications, and an accelerated return to everyday activities lead to better patient outcomes as well as a more sustainable healthcare framework
Consequently, both public authorities and private organizations are starting to invest additional resources in advancing and spreading these methods
In addition, the mindset and traditions in the surgical field are experiencing a significant evolution
A prioritization of enduring learning, joint multidisciplinary engagement, and rigorously tested practices is crafting a climate where innovation is simultaneously supported and demanded.
This cultural transformation is poised to expedite click to read more the integration of novel techniques and breakthrough technologies, ultimately delivering comprehensive benefits to patients everywhere.
Final Analysis: A Fundamental Redefinition in Patient-Centric Surgical Practices.
The evolution of these advanced surgical methods reflects a transformative shift in the approach to delivering surgical care.
These techniques have pioneered a new frontier in surgical care by focusing on precision, tissue-sparing approaches, and muscle conservation, thereby significantly improving patient results.
From the origin of laparoscopic methods to the state-of-the-art merger of robotics with artificial intelligence, the journey reflects unremitting innovation and an enduring pursuit of perfection.
For patients, the expected benefits include decreased pain, faster return to daily activities, and a higher level of life quality.
For surgeons and healthcare providers, the challenge is to master these innovative techniques, invest in cutting-edge technology, and cultivate a culture of constant advancement.
With the steady march of scientific research and technology, the potential for new innovations in these surgical techniques remains impressive.
Future surgical paradigms will focus on patient-centric care, with devices and procedures designed to improve, not impair, the body’s natural capabilities.
Looking forward, the synthesis of high-tech imaging, robotics, and regenerative medicine is expected to herald new frontiers in care that prioritize the patient.
The continual evolution of surgical techniques demonstrates the medical community’s steadfast commitment to innovation, ensuring safety, and striving for better outcomes.
As individualized healthcare becomes the norm, micro-invasive and muscle-sparing techniques emerge as symbols of a future where interventions are less traumatic and patient outcomes are significantly improved.
The journey presses on, and with each new discovery, we move nearer to a future where surgery is redefined from being associated with pain and lengthy recovery to serving as a conduit for revitalized health and energy.
References and Further Reading.
Clinical Studies and Reviews: A multitude of peer-reviewed studies published in journals such as the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education offer robust data on patient outcomes and the merits of these techniques.
Expert Interviews: Testimonies from prominent surgeons such as Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen offer valuable insights into both the advantages and the practical challenges of these techniques.
Technological Innovations: State-of-the-art progress in robotic-assisted surgery and augmented reality in the operating room is highlighted in contemporary publications and at international conferences.
These innovative techniques have set a new standard in patient-centric care. Emphasizing precision, minimizing tissue disruption, and preserving muscle function, they lead to improved clinical outcomes and a more positive patient journey.
As cutting-edge technologies evolve and gain traction in medical practices worldwide, the future of surgical care is anticipated to bring even more pronounced benefits to patients everywhere.
Within this dynamic field, an unwavering commitment to continuous progress is the genuine measure of success—a pledge that will reimagine surgical care for generations.
 Hallie Eisenberg Then & Now!
Hallie Eisenberg Then & Now! Kelly McGillis Then & Now!
Kelly McGillis Then & Now! Jenna Von Oy Then & Now!
Jenna Von Oy Then & Now! Lucy Lawless Then & Now!
Lucy Lawless Then & Now!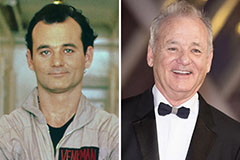 Bill Murray Then & Now!
Bill Murray Then & Now!